New guidance from the American Academy of Neurology (AAN) concludes that closure of a common heart defect called a patent foramen ovale (PFO) may be recommended for some people who have had a stroke.
The updated practice advisory is published in the April 29, 2020, online issue of Neurology®, the medical journal of the American Academy of Neurology.
Closure may be considered for some people under age 60 to help prevent a second stroke, according to the practice advisory, which is endorsed by the American Heart Association/American Stroke Association, the Society for Cardiovascular Angiography and Interventions and the European Academy of Neurology.
A PFO is a channel between the right and left sides of the heart. All infants have this small flap-like opening between the two sides. In most people, this channel closes on its own by adulthood. But for about one in four people, it remains open. “
It’s important to note that having a PFO is common, and that most people with PFO will never know they have it because it usually does not cause any problems,” said study author Steven R. Messé, M.D., of the Perelman School of Medicine at the University of Pennsylvania, and a Fellow of the American Academy of Neurology. “However, while there is generally a very low risk of stroke in patients with PFO, in younger people who have had a stroke without any other possible causes identified, closing the PFO may reduce the risk of having another stroke better than medication alone.”
In PFO closure, doctors use a catheter to place a device in the channel between the right and left sides of the heart to prevent blood flow.
For the practice advisory, clinical experts carefully reviewed the available evidence about stroke prevention in patients with a PFO who had already had an ischemic stroke, which is a stroke caused by a blockage in a blood vessel leading to reduced blood flow.
When considering PFO closure in people who have had a stroke, the practice advisory recommends that doctors with expertise in stroke to first rule out causes other than the PFO, such as hardening or a tear of the blood vessels, heart disease including abnormal heart rhythms, or an increased risk for forming clots, to ensure that PFO is the most likely cause of stroke. The practice advisory does not recommend PFO closure if another higher risk cause of stroke is identified. The advisory also recommends that patients considering closure have a consultation with an expert in PFO closure, to ensure that the procedure can be safely performed.
The practice advisory states for people younger than 60 years old who have had a stroke thought to be caused by a PFO and no other cause, doctors may recommend closure of the PFO after discussing the potential benefits, including a 3.4% reduction in the risk of a second stroke in five years, as well as the potential risks, such as a 3.9% chance of procedural complications and an increased risk of an abnormal heart rhythm called atrial fibrillation of 0.33% per year.
“The risk of a second stroke in people with PFO and no other possible causes of stroke is very low, approximately 1% per year while being treated with just medication alone,” said Messé. “Also, it is difficult to determine with absolute certainty that the PFO is the cause of a person’s stroke. So it is important that people with PFO are educated about the benefits and risks of PFO closure.
Transcranial Doppler ultrasonography (TCD) from Delica EMS-9D has been demonstrated to detect right-to-left shunting with sensitivity and specificity. It is noninvasive and fairly easy to use compared with TEE..This clinic use requires the administration of agitated saline after which the patient performs a valsalva maneuver. The test is positive for right to- left shunt if a shower of high signal material (air) is detected in the MCA by TCD 5 to 10 seconds after the intravenous injection of 10 mL of agitated saline. If this shower of air emboli is detected after a minute of injection, it might indicate the presence of a pulmonary shunt; a diagnosis that cannot be obtained by TEE as well.
Reference: Practice advisory update summary: Patent foramen ovale and secondary stroke prevention
 Delica Distributor Meeting in AmsterdamDelica Medical organized an international distributor meeting in Amsterdam, the Netherlands from April 2nd to 3rd. Nearly 28 participants from Europe and some other countries took part in this meeting.
Delica Distributor Meeting in AmsterdamDelica Medical organized an international distributor meeting in Amsterdam, the Netherlands from April 2nd to 3rd. Nearly 28 participants from Europe and some other countries took part in this meeting.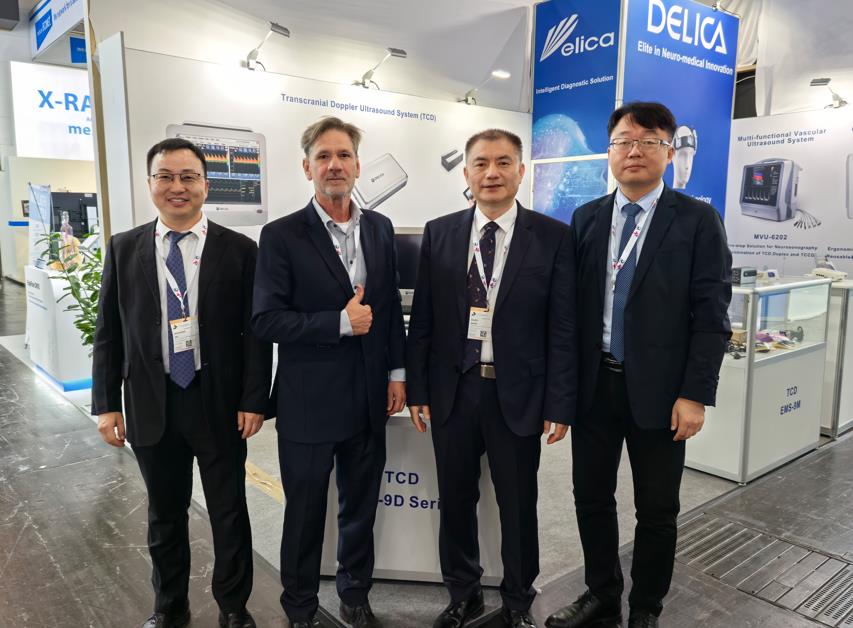 Delica in Medica 2024From November 11 to 14, 2024 Dusseldorf International Medical and Medical Device Fair (MEDICA) was held in Dusseldorf Exhibition Center, Germany.
Delica in Medica 2024From November 11 to 14, 2024 Dusseldorf International Medical and Medical Device Fair (MEDICA) was held in Dusseldorf Exhibition Center, Germany. DELICA made a wonderful appearance in MEDICAFrom November 13 to 16, 2023 Dusseldorf International Medical and Medical Device Fair (MEDICA) was held in Dusseldorf Exhibition Center, Germany.
DELICA made a wonderful appearance in MEDICAFrom November 13 to 16, 2023 Dusseldorf International Medical and Medical Device Fair (MEDICA) was held in Dusseldorf Exhibition Center, Germany.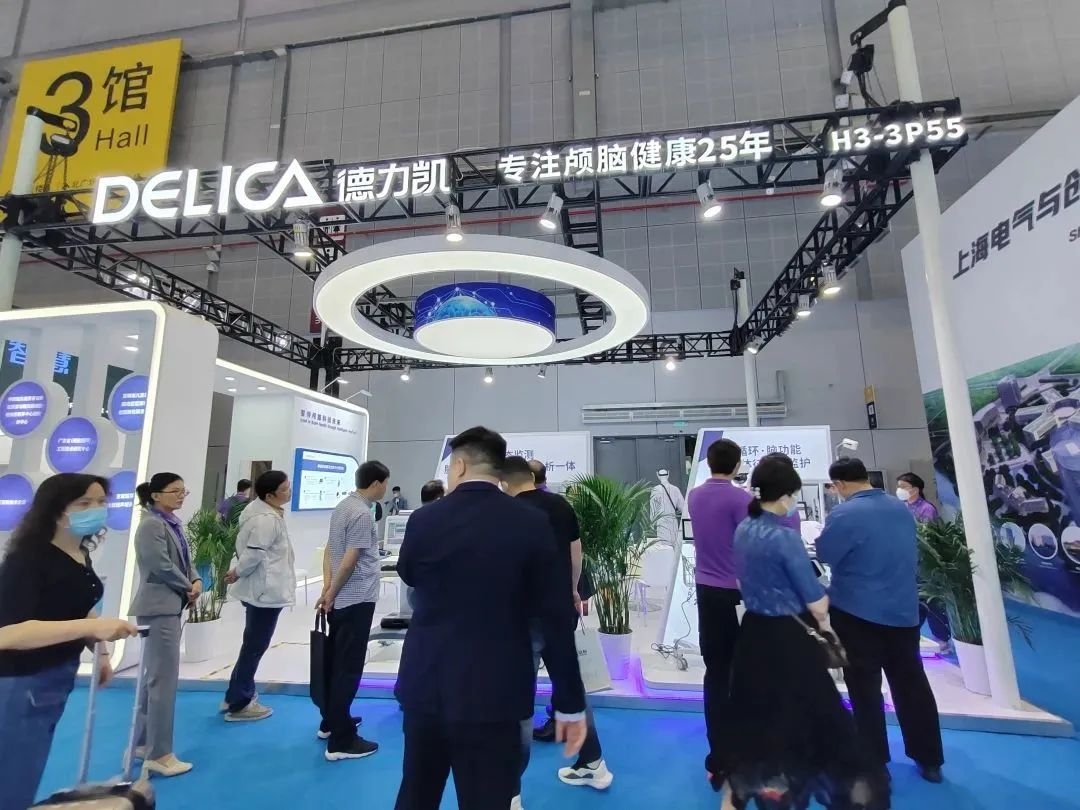 DELICA made a wonderful appearance in the 87th CMEFFrom May 14 to 17, 2023, the 87th China International Medical Equipment Fair (CMEF) was grandly opened in Shanghai National Convention and Exhibition Center. Nearly 5,000 elite enterprises gathered in the event, covering more than 320,000 square meters, nearly 100 conferences and forums, hundreds of special activities, and tens of thousands of products. Industry celebrities and elite gathered in the scene, innovative technology and cutting-edge academic blend here, infinite business opportunitie
DELICA made a wonderful appearance in the 87th CMEFFrom May 14 to 17, 2023, the 87th China International Medical Equipment Fair (CMEF) was grandly opened in Shanghai National Convention and Exhibition Center. Nearly 5,000 elite enterprises gathered in the event, covering more than 320,000 square meters, nearly 100 conferences and forums, hundreds of special activities, and tens of thousands of products. Industry celebrities and elite gathered in the scene, innovative technology and cutting-edge academic blend here, infinite business opportunitie Delica Medical Workshop at Haga Teaching hospitalDelica Workshop at Haga Teaching hospital. Thank you Dr Ruud Keunen for the wonderful lectures!
Delica Medical Workshop at Haga Teaching hospitalDelica Workshop at Haga Teaching hospital. Thank you Dr Ruud Keunen for the wonderful lectures! Delica Medical Participated in CARNET 2022Shenzhen Delica Medical Equipment Co., Ltd. (Delica) Participated in the Cerebrolvascular Research Network (CARNet) meeting in Leicester, UK during 27 th – 29th October 2022.
Delica Medical Participated in CARNET 2022Shenzhen Delica Medical Equipment Co., Ltd. (Delica) Participated in the Cerebrolvascular Research Network (CARNet) meeting in Leicester, UK during 27 th – 29th October 2022. Delica Medical at European Stroke (ESOC) MunichShenzhen Delica Medical Equipment Co., Ltd. (Delica) Participated in the European Stroke (ESOC) 2023 Munich, a lot of interest in High Tech Robotic Probes on Delica TCD
Delica Medical at European Stroke (ESOC) MunichShenzhen Delica Medical Equipment Co., Ltd. (Delica) Participated in the European Stroke (ESOC) 2023 Munich, a lot of interest in High Tech Robotic Probes on Delica TCD Robotic TCD monitoring during TAVI ProcedureTranscranial Doppler(TCD)is a useful diagnostic tool that can be used at bedside to evaluate patients with cerebrovascular disease. As we all know the clinical application from the AAN’s guideline such as Sickle cell screening
Robotic TCD monitoring during TAVI ProcedureTranscranial Doppler(TCD)is a useful diagnostic tool that can be used at bedside to evaluate patients with cerebrovascular disease. As we all know the clinical application from the AAN’s guideline such as Sickle cell screening The 23rd China International HI-TECH FAIRThe 23rd China International HI-TECH FAIR took place in Shenzhen on 27th-29th Dec, 2021 with the theme of advancing high-quality development and fostering a new development pattern.
The 23rd China International HI-TECH FAIRThe 23rd China International HI-TECH FAIR took place in Shenzhen on 27th-29th Dec, 2021 with the theme of advancing high-quality development and fostering a new development pattern. MEDICA 2021, Delica Medical showcases its innovative product .Delica Showcasing Their Latest Generation Product and Technology innovation.
MEDICA 2021, Delica Medical showcases its innovative product .Delica Showcasing Their Latest Generation Product and Technology innovation.